Description
Find out how CMS’s decision requiring hospital outreach programs to report lab payment data starting next year will impact the second round of Medicare rate-setting under PAMA.
Significantly, CMS announced as part of its CY 2019 Physician Fee Schedule final rule that virtually all hospital outreach labs that meet the volume thresholds will be required to report private-payer payment data under PAMA (January 1 to June 30, 2019). Moreover, CMS is permitted to impose civil monetary penalties against labs required to report data, but fail to do so.
Meantime, the American Clinical Laboratory Association has stated it intent to appeal a federal judge’s dismissal of its lawsuit over Medicare’s new market-based pricing system. Finally, the court ruling has accelerated industry lobbying reports on Capitol Hill to amend PAMA.
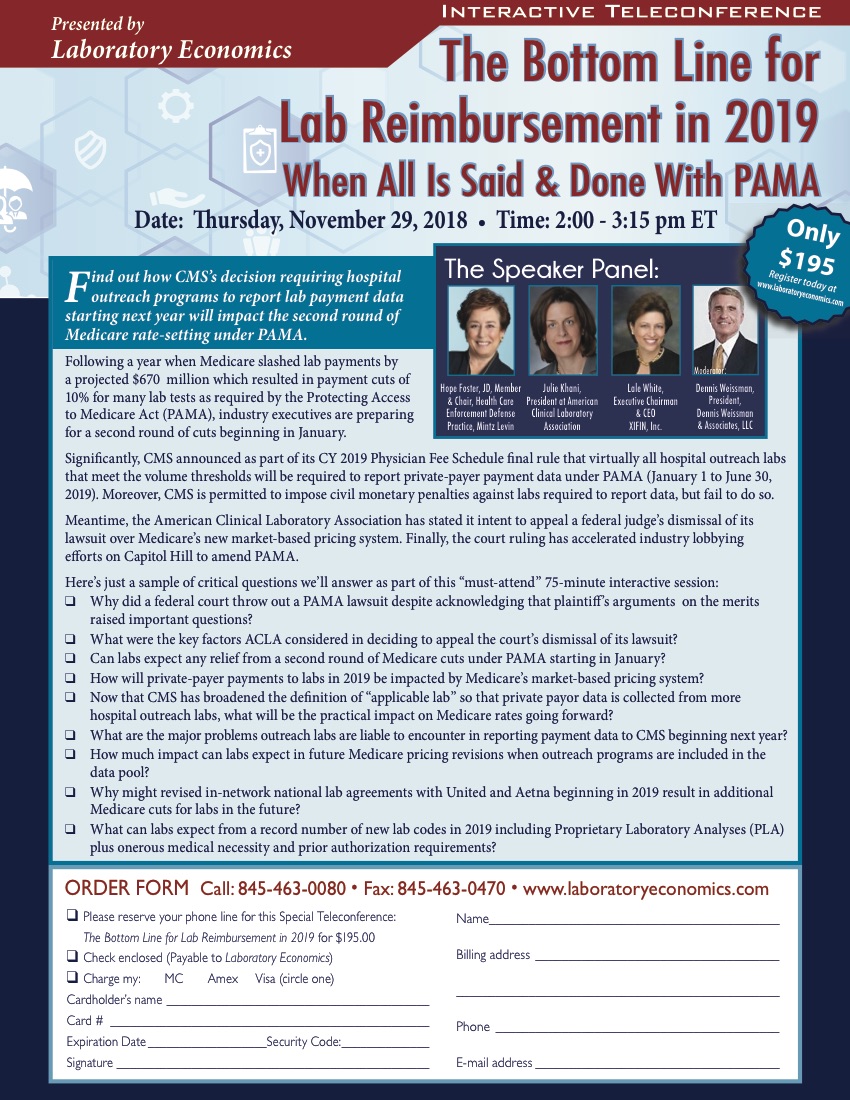
SPEAKER PANEL

Hope Foster
Member & Chair, Health Care Enforcement Defense Practice, Mintz Levin

Julie Khani
President at American Clinical Laboratory Association

Lale White
Executive Chairman & CEO XIFIN, Inc.

Dennis Weissman
President, Dennis Weissman Associates, LLC