PAMA Delay Included in New Spending Law
PAMA Delay Included in New Spending Law
On Feb. 3, President Trump signed into law a $1.2 trillion spending
package. Included in the Consolidated Appropriations Act of 2026 is a freeze in Medicare CLFS rates through December 31, 2026. In addition, the new law modifies the private-payer data collection and reporting period for labs. Labs will now have to collect their private-payer payment data from January 1 – June 30, 2025, and report it to CMS between May 1, 2026 – July 31, 2026. CMS will use this data to calculate CLFS rates for 2027. “This is welcome relief, but what we really need is permanent reform,” says Erin Morton, Washington Representative for the National Independent Laboratory Association (NILA) and Partner at CRD Associates (Washington, DC).
Morton says NILA will continue to lobby for the broader PAMA reforms contained in the RESULTS Act. In particular, Morton says that there is concern that a minority of labs will report their private-payer payment data for 2025 to CMS by July 31, 2026. This could lead to a scenario similar to the first PAMA survey, which was skewed toward pricing data submitted by the national labs.
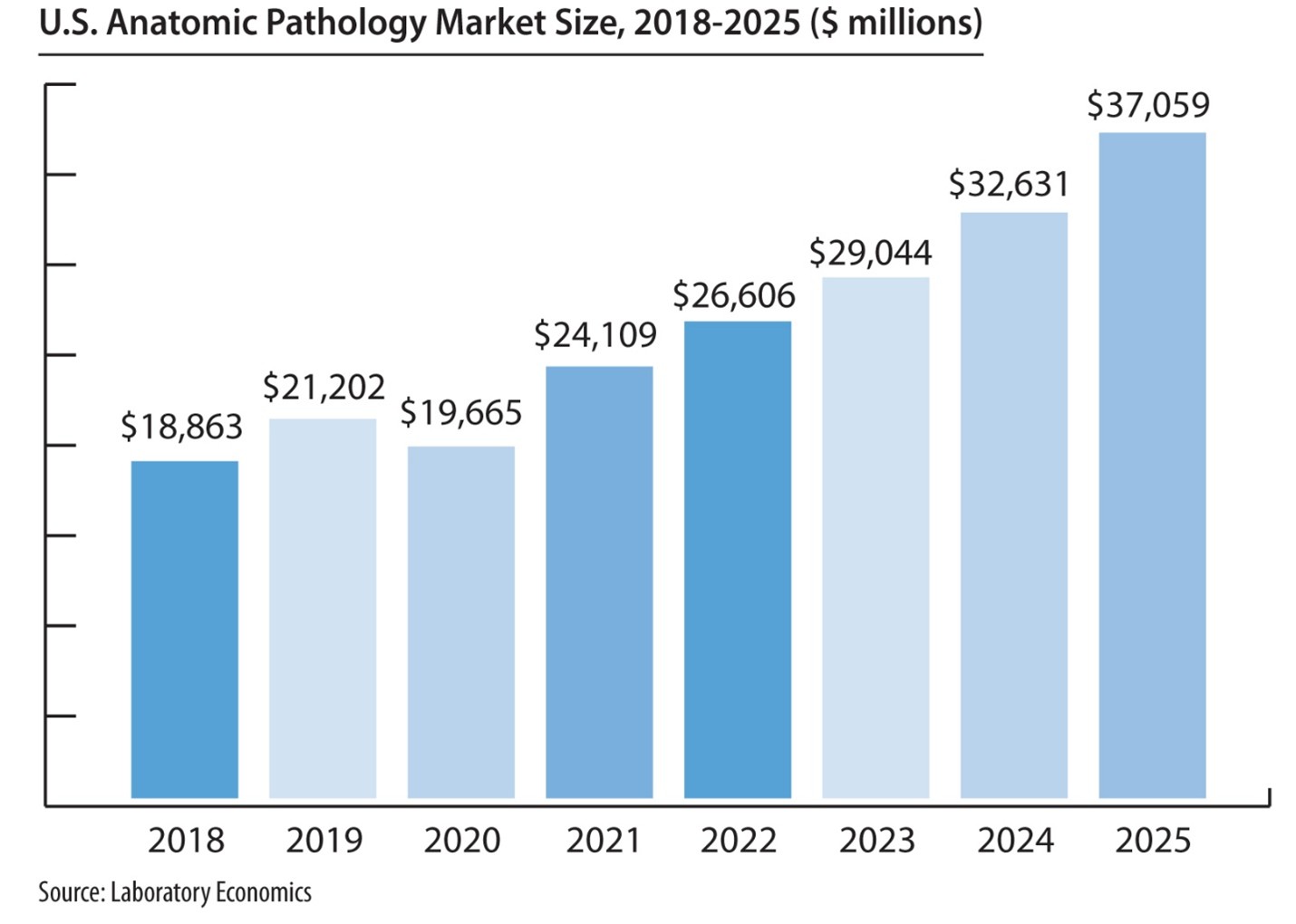
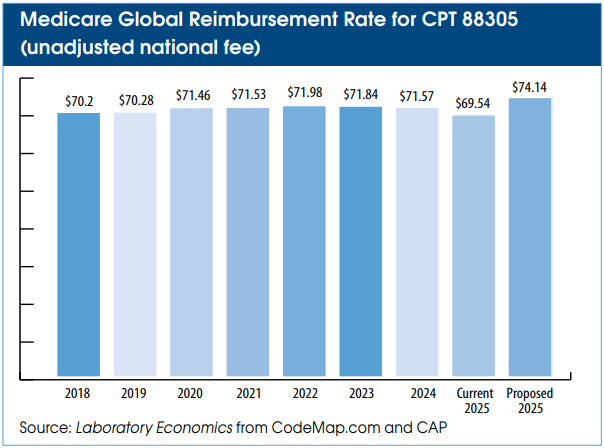
The result was three straight years (2018-2020) of 10% rate cuts to most test codes on the CLFS.
If passed, the RESULTS Act would remove the PAMA reporting burden from labs. Instead, pricing data would be supplied to CMS from an independent nonprofit entity (e.g., The FAIR Health
Database). This would ensure that pricing data from all labs (independents, hospitals and POLs) was accurately represented.
ACLA President Susan Van Meter says the next best chance for getting the RESULTS Act passed into law would be to have it inserted into a bigger budget bill expected to be introduced at the end of the year.
However, lab policy expert Dennis Weissman, says that passing the RESULTS Act into law will be difficult because it is likely to have a projected 10-year cost of billions of dollars. Furthermore, Weissman notes the new PAMA reporting period was only delayed by three months. Once the reporting process begins on May 1, it may be hard to stop, notes Weissman, who heads Dennis
Weissman & Associates (Falls Church, VA).
PAMA Policies included in Consolidated Appropriations Act of 2026 (Section 6226):
- Delays PAMA rate cuts of up to 15% on about 800 tests and freezes the Clinical Laboratory Fee Schedule (CLFS) through December 31, 2026.
- Updates private payer data CMS will use to set CLFS rates for 2027 by shifting the data collection period to January 1 – June 30, 2025 (previously it was January 1 – June 30, 2019).
- Moving to an updated data collection period should allow for improved data reporting, as 2019 data was inaccessible to many laboratories.
- CMS is preparing a laboratory data reporting educational campaign to inform hospital outreach, independent and physician office laboratories (POLs) of the requirement to report 2025 data.
- Shifts the data reporting period to May 1, 2026 – July 31, 2026, after which CMS will calculate volume-weighted median private-payer rates to set CLFS rates effective January 1, 2027.
Which labs must report?
“Applicable laboratories” include those that bill Medicare Part B under their own National Provider Identifier (NPI) numbers. These include independent labs, hospital outreach labs and physician office labs that received at least $12,500 of Medicare revenues from the CLFS between January 1 and June 30, 2025. Hospital outreach labs must report if they bill Medicare Part B on Form CMS1450 under type of bill 14x. This means that approximately 3,000 hospitals with CLFS revenue are required to report.
Which data must be reported?
Applicable labs must report their private-payer payment data for nearly all test codes (~1,500 lab tests) on the CLFS to CMS beginning May 1, 2026, through July 31, 2026. The required data includes private-payer volume and rates from final claims paid between January 1 and June 30, 2025. CMS will use this information to calculate a volume-weighted median rate for each CPT code and to set new Medicare CLFS rates for 2027-2029. CLFS rates for 2027-2029 will be subject to a maximum annual cut of 15% per year.
What are the penalties for not reporting?
Failure to report could result in a penalty of up to $10,000 per day. After the first PAMA survey, CMS never set up a system for tracking non-reporting labs and instituting civil monetary policies. However, the agency’s leniency may not continue for the next PAMA reporting period. More information on PAMA reporting is available here.